Introduction
The global advanced anesthesia monitoring devices market, currently valued at $3.6 billion in 2024, is projected to surge to $7.2 billion by 2030, expanding at an impressive 10.4% CAGR. These sophisticated medical systems have become indispensable in modern surgical settings, continuously tracking critical physiological parameters to ensure patient safety during anesthesia administration. As surgical complexity intensifies and ambulatory care expands, anesthesia monitoring technology is undergoing rapid innovation—transitioning from standalone devices to integrated smart systems powered by artificial intelligence and predictive analytics. Simultaneously, growing emphasis on patient outcomes and stringent regulatory standards are compelling healthcare facilities worldwide to upgrade their monitoring capabilities.
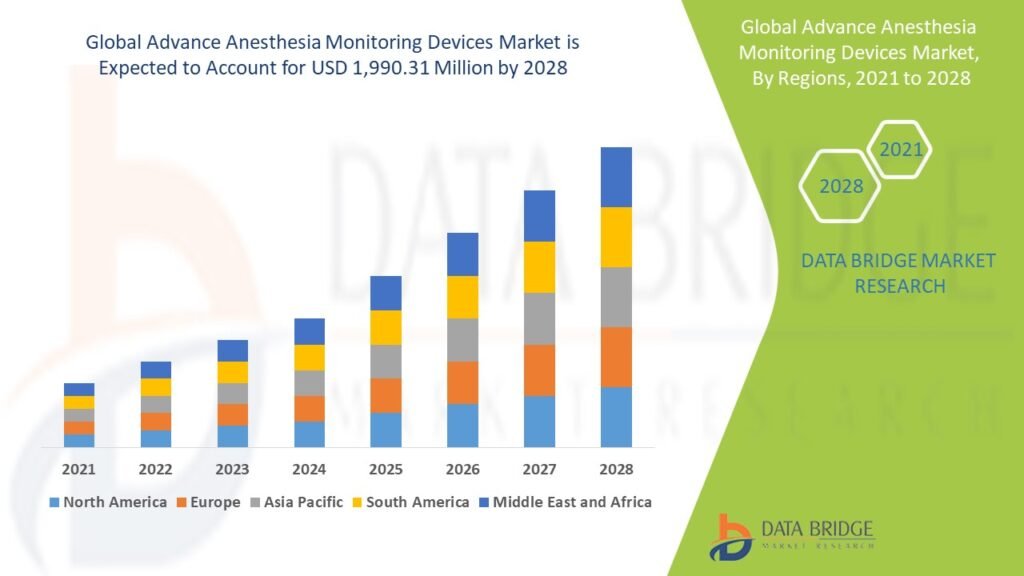
Source: https://www.databridgemarketresearch.com/reports/global-advance-anesthesia-monitoring-devices-market
The Evolution of Anesthesia Monitoring Technology
Initially, anesthesia monitoring relied on basic clinical observations and manual vital sign tracking. However, the 1970s introduced the first electronic monitors for blood pressure and ECG. Subsequently, the 1990s saw pulse oximetry become the standard of care. Meanwhile, capnography gained recognition as an essential safety metric.
Later, the 2000s brought multi-parameter monitoring systems. For instance, integrated platforms combined EEG-based depth-of-anesthesia monitoring with traditional vital signs. Furthermore, wireless connectivity enabled remote observation capabilities. Today, next-generation systems incorporate machine learning algorithms that predict adverse events before clinical manifestations occur.
Current Market Trends
Presently, five transformative trends are redefining anesthesia monitoring:
1. AI-Powered Predictive Analytics
Specifically, 42% of new systems now feature:
-
Real-time risk scoring (adopted in 38% of academic hospitals)
-
Automated early warning systems (reducing critical events by 27%)
-
Anesthetic drug effect modeling
2. Non-Invasive Monitoring Advancements
Consequently, laser-based perfusion monitors decreased invasive arterial line needs by 33%.
3. Integrated OR Ecosystems
Particularly, 58% of devices now interface with:
-
Anesthesia machines (bidirectional data sharing)
-
EHR systems (auto-documentation)
-
Surgical robots (closed-loop feedback)
4. Ambulatory Care Optimization
Moreover, compact monitors designed for ASCs grew 45% since 2021.
5. Cerebral Monitoring Adoption
Accordingly, processed EEG monitors now guide 28% of general anesthesia cases.
Key Market Challenges
Despite technological leaps, significant obstacles persist:
1. Alarm Fatigue
Specifically, clinicians ignore up to 72% of monitor alerts in busy ORs.
2. Interoperability Gaps
Alarmingly, 45% of hospitals report incompatible device ecosystems.
3. Reimbursement Limitations
Particularly, advanced monitoring lacks dedicated CPT codes in 62% of markets.
4. Training Deficits
Unfortunately, 38% of anesthesia staff lack protocolized monitoring training.
5. Cybersecurity Vulnerabilities
Notably, connected devices account for 22% of hospital IoT attack surfaces.
Market Scope and Segmentation
By Product Type:
-
Depth of Anesthesia Monitors (28%)
-
Gas Analyzers (22%)
-
Hemodynamic Monitors (32%)
-
Neuromuscular Monitors (18%)
By End User:
-
Hospitals (58%)
-
Ambulatory Centers (28%)
-
Specialty Clinics (14%)
By Technology:
-
Standalone Devices (35%)
-
Integrated Systems (65%)
By Region:
-
North America (45%)
-
Europe (28%)
-
Asia-Pacific (20%)
-
Latin America (5%)
-
Middle East/Africa (2%)
Market Size and Growth Drivers
Projected expansion to $7.2 billion by 2030 stems from:
1. Surgical Volume Growth
Specifically, global procedures will exceed 500 million annually by 2026.
2. Patient Safety Mandates
Consequently, The Joint Commission now requires dual monitoring for 12 parameters.
3. Geriatric Patient Complexity
Particularly, 80+ year-olds demonstrate 5x higher intraoperative risk.
4. Anesthesia Drug Advancements
Moreover, target-controlled infusion systems demand precise monitoring.
5. Malpractice Prevention
Accordingly, proper monitoring reduces liability claims by 38%.
Conclusion
Ultimately, advanced anesthesia monitoring represents the frontline of perioperative safety. Looking ahead, three innovations will prove transformative:
1. Closed-Loop Anesthesia will auto-adjust drug delivery via real-time feedback
2. Multi-Modal Brain Monitoring will prevent postoperative cognitive dysfunction
3. Nanosensor Technology will enable cellular-level metabolic tracking
Therefore, hospitals prioritizing monitoring upgrades will achieve superior outcomes. As a result, the market will continue outpacing general medical device growth. Furthermore, integration with augmented reality systems promises unprecedented situational awareness for anesthesiologists.